Dr Annette Barrett and the DRS4DRS service
Posted on December 22, 2023

Content warning: Please be aware this story contains reference to suicide, which might be distressing for some, particularly those with lived experience. If you need help or would like to talk to someone, please call Lifeline on 13 11 14 or the Suicide Call Back Service on 1300 659 467.
Dr Annette Barratt has practised as a GP in and around Hobart for the past 40 years.
A former state Chair of the Royal Australian College of General Practitioners and current Vice President of the Australian Medical Association in Tasmania, she is also a commissioner with the Voluntary Assisted Dying Commission.
Annette has a long-standing interest in doctors’ health and wellbeing, which has led to her appointment as state medical director of the not-for-profit DRS4DRS health service – a volunteer position.
Why do doctors need their own medical service?
A lot of GPs manage their own health, often poorly. And a lot of specialists manage their own health. Doctors often don’t go to other doctors and even when they do consult a colleague, it’s via a ‘corridor’ consultation rather than a formal appointment.
General practice can be a very isolating profession and unfortunately, GPs often don’t ask for help. They suffer in silence.
Doctors have been taught all the way through their training that the buck stops with them. It’s very hard then to go and ask for help. And doctors can see it as a weakness, especially to admit mental health issues or addiction issues. They see it as a failure. Whereas in reality, it’s just being human.
There’s also a great fear of being reported to AHPRA (the Australian Health Practitioner Regulation Agency) and being told you can’t practise – so instead of reaching out for help, people soldier on until it becomes too hard. And then unfortunately, they often self-harm in one way or another. We know the suicide rate amongst medical professionals is high – particularly, unfortunately, among young female GPs. They feel unsupported and isolated. And that’s what we’re trying to avoid.
What effect has the COVID-19 pandemic had on health professionals’ support needs?
General practice is different to working in a hospital, where you’re never alone. In general practice it’s just you and your patient in your room, which is more isolating. The pandemic made it even worse because doctors were working from home, so they never even had the support of their own practice.
What can healthcare practices do to support the health and wellbeing of their staff?
When I was principal owner at a practice in Bridgewater, we had things in place to protect our doctors. We would not allow any of our doctors to work full time; no-one would work more than four days a week. We encouraged them to do other things to diversify, to make sure that they weren’t burning out. And we had lunch together every single day – every doctor, the reception staff, the nursing staff, as a way of building support for each other.
I’d say form communities within your practices, and form communities within your area, to be able to support each other. That could be across disciplines – it doesn’t have to be just GPs.
What can healthcare providers do to support themselves, and each other?
Encourage each other to have a healthy work-life balance; look out for each other; watch whether your colleague is not coping. And have the courage to go and talk to them. We know that talking is the most important way of picking up problems.
I’d also really encourage doctors to do the DRS4DRS training. Even if they don’t want to be on our volunteer roster – it’s free training, it only takes a couple of hours, but it gives incredible insight into the issues doctors are facing and how to manage caring for your peers. Then if they want, they can join my roster of doctors taking calls from colleagues in need. They can commit as little or as much time as they want – some doctors do regular weeks on call; others may only have time to do a few days per year. It all helps.
What system-level changes are needed?
We’ve got to change the expectation that doctors are perfect, and that doctors are seen as superhuman. We’ve got to keep the dialogue about the fact that doctors are human, and have the same problems as everyone else.
Also that mental health issues don’t prevent a doctor from being a good doctor. People are frightened that if they identify as having a mental health issue, they’re going to be stopped from practising. And that’s not accurate.
And that’s the thing that we need to get out there – people seeking help early is not going to stop them being a good doctor. In many ways, it is going to make them a better doctor.
What is DRS4DRS?
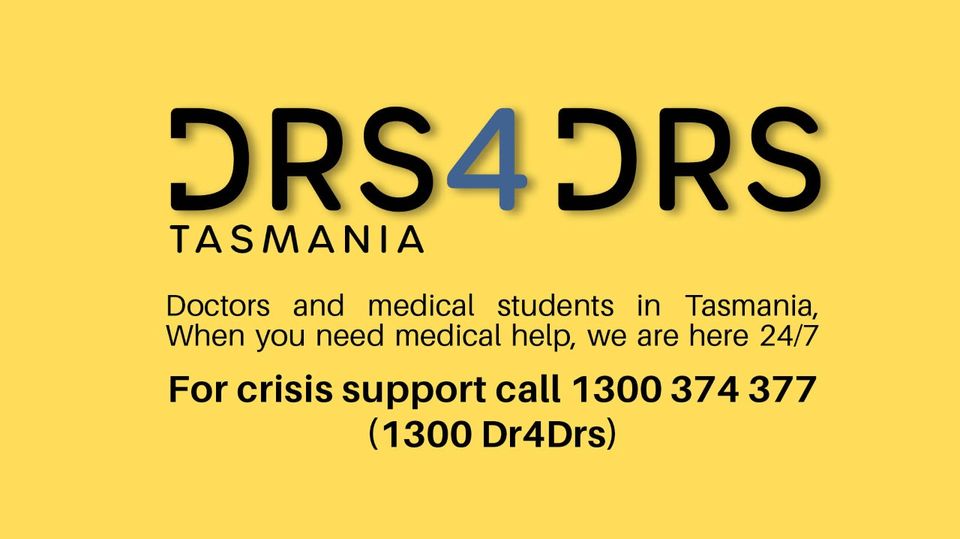
DRS4DRS is a free and confidential health and wellbeing service available to doctors, medical students and their families throughout Australia.
Each state – including Tasmania – has a 24/7 helpline (1300 374 377 in Tasmania) staffed by senior GPs and other doctors who talk to callers about their concerns – physical and mental – and provide them with advice on what steps to take next.
DRS4DRS is funded by the Medical Board of Australia and – locally – the Tasmanian Government, but operates independently. It is administered by the Australian Medical Association.
Want to know more? Go to www.ama.com.au/drs4drs/tas
This story features in Issue 17 of our Primary Health Matters magazine. Click here to read the rest of the issue.